The vulva is the external part of the female genitalia . Apart from the vaginal opening ( vestibule ) includes large and small lips - skin structures that protect the vaginal opening - and the clitoris, formed by very sensitive tissue that swells to the passage of blood as a result of sexual stimulation.
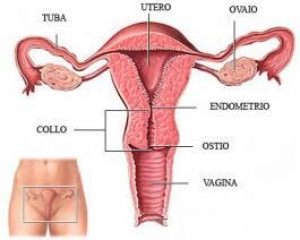
The vagina is a sort of channel (it is also called the " birth canal " ) that connects the vulva and cervix .
The inner wall of this channel is lined by a squamous epithelium below which there are muscles , connective tissue, lymph nodes and blood vessels. In proximity of the vaginal opening are the Bartholin's glands , one on each side , which produce a liquid lubricant during sexual intercourse .
All the cells that make up the vulva and vagina can theoretically give rise to a tumor, although the most common ones involve the labia , clitoris and while those of other regions are rarer.
How widespread is
Tumors of the vulva and vagina are not very common and account for about 5 percent of all cancers affecting the female genital tract .
According to the data AIRTUM (Italian Association of Cancer Registries ) of more than 2.2 million people living with a diagnosis of cancer, less than 9000 are those who have received a diagnosis of cancer of the vulva and vagina.
The disease can affect people of all ages , but in most cases the diagnosis relates to women around 70 years old and very rarely women under the age of 40 years.
Who is at risk
The age is a risk factor for cancers of the vulva and vagina that usually affect women over 50 years ( half of them over 70 ), but the risk increases even in the event of improper lifestyles : in smokers , for example , doubles the risk of cancer of the vagina and increases that of cancer of the vulva .
Some viruses may be linked to the risk of cancer of the vulva and vagina : Women who are infected with papillomavirus (only some viral types , are also responsible for other cancers ) are more at risk, as well as those positive for the HIV virus that weakens the immune system.
Other conditions, such as vaginal adenosis , the presence of cervical cancer or pre-cancerous lesions and vaginal irritation are associated with increased risk of cancer of the vagina, while the risk of cancer of the vulva is affected by the presence of intraepithelial neoplasia vulvar (VIN, a pre-cancerous condition ) , other cancers of the genital lichen sclerosus or melanoma or atypical moles in other regions of the body.
It was also noted that the vaginal cancer occurs more frequently than normal in the daughters of women who took diethylstilbestrol (DES) , a drug used between 1940 and 1970 to prevent miscarriage.
Types
Vulva and vagina can be affected by different types of cancer. The most common is undoubtedly the squamous cell carcinoma (7 of 10 vaginal cancers and the majority of those vulvar ) in the vagina this tumor is most common in the area close to the cervix and usually originates from a pre-cancerous lesion ( VAIN , English vaginal intraepithelial neoplasia ) that may later become a tumor, in a process that can last several years.
In squamous cell carcinoma of the vulva can also be kind of warty and take on the appearance of a wart to slow growth.
When instead the tumor arises from a glandular cell , takes the name of adenocarcinoma , another type of cancer that affects the vulva (8 out of 100 cases , in particular cells of Bartolini ) and vagina (15 cases out of 100 ) .
Less common , but still present in the vulva and vagina are also melanomas (6 percent of vulvar cancers , especially in the clitoris and the labia minora , and 9 percent of those vaginal ) , tumors that originate from cells that produce pigments that color the skin, and sarcomas ( 2 percent of vulvar cancers and 4 percent of those specimens) that are derived from the cells of muscle and connective tissue.
Symptoms
Tumors of the vulva and vagina may be completely asymptomatic in the early stages at least , or give rise to general symptoms attributable to other non- oncological diseases .
In the case of suspicious symptoms , however, it is best to consult your doctor or gynecologist. More than 80 percent of women with invasive cancer of the vagina shows bleeding ( often after sexual intercourse ), or abnormal vaginal discharge , pain during intercourse and , in more advanced cases , even discomfort when urinating , constipation and pelvic pain continuously.
For cancer of the vulva symptoms are a little ' different in the case of invasive squamous cell carcinoma of the early stages the symptoms are changes in the appearance of an area of ??skin of the vulvar region concerned, which appears thinner , or more red or darker than the surrounding areas.
As the disease progresses , the skin is modified further by assuming the appearance of a nodule red or white with a rough surface and in some cases there are also itching, pain or burning, and abnormal losses not related to the menstrual cycle or wounds that do not heal for long periods .
As for melanoma from other regions of the body , even the vulva looks like a mole which changes in appearance or appear de novo and that has characteristics typical of the malignant ( asymmetry , ragged edges , uneven color and diameter greater than 6 mm ) .
Prevention
To prevent cancer it is important to try to avoid substances and behaviors that increase the risk , a rule that applies also for cancers of the vulva and vagina.
In these cases it is important to avoid smoking and should try to avoid infection with papillomavirus , a virus that is contracted through sexual intercourse with an infected person and sexual risk behaviors ( such as a high number of partners, early onset of ' sexual activity etc.) .
The regular gynecological check-ups can prove to be crucial in the prevention of cancers of the vulva and vagina as possible to find out any pre-cancerous lesions in the years that could turn into a tumor.
Once identified through examinations and tests specific VIN ( vulvar intraepithelial lesions ) and VAIN ( vaginal intraepithelial lesions ) can be treated in the most appropriate way to eliminate the risk that evolve into cancer .
Finally, a monthly self-examination of the vulva , easily practicable thanks to a mirror , can help identify early changes suspects ( in , redness, etc.) to bring to the attention of the physician.
Diagnosis
The diagnosis of cancer of the vulva and vagina begins with a gynecological examination during which the specialist assesses symptoms , make a thorough examination of the genital area , collects information on medical history and family and , if deemed necessary, carry out or require further examination .
The colposcopy , for example, is a rather quick and painless examination that allows the physician to observe in detail the cells lining the vagina and cervix and to highlight any anomalies.
In the case of areas "suspicious" proceed with the biopsy , that is, the removal of some cells to be analyzed under the microscope, which allows you to establish or exclude with certainty the presence of cancer of the vagina.
Even for cancer of the vulva diagnosis is made based on the analysis of cytological biopsy.
Once diagnosed with certainty the tumor , we proceed with other tests to see if the disease has spread to other organs typically use X-rays , MRI, CT , PET and some tests " endoscopic " as cystoscopy , which analyzes the bladder through a tube to which is fixed a probe that allows to illuminate and view the area and, if necessary , also to take samples of tissue , or proctoscopy that uses the same technique to the rectum.
Evolution
The stage of cancer of the vulva and vagina , which indicates how the disease is spread , is assigned using the FIGO staging system (International Federation of Gynecology and Obstetrics ) and combined with the dell'AJCC (American Joint Committee on Cancer ) and is based on the criteria " TNM " where T refers to the extension of the disease, the involvement of lymph nodes N and M in the presence of metastases.
How to care
The choice of treatment to be carried out in the case of cancer of the vulva and vagina depends on numerous factors , such as type , location and dissemination of the disease , age and physical condition of the patient.
Surgery is an important treatment option and the intervention can be more or less invasive as appropriate : surgery that " vaporizes " cancer cells , for example , is effective for pre-cancerous lesions both vulvar ( VIN ) both vaginal ( VAIN ) , but it is not suitable for the treatment of invasive tumors .
In those cases we resort to traditional surgery that involves the removal of the tissues affected by the tumor and, if necessary , also the subsequent reconstruction of the removed parts .
The reconstruction of the vagina allows women to have sex after surgery , while the reconstruction of the external genitalia ( vulva ) is a function primarily psychological and often helps women feel less uncomfortable in intimate life .
In general, after an intervention of vulvectomy ( removal of all or part of the vulva ) is very difficult for a woman is able to orgasm since the external genitals , especially the clitoris, have a key role in female pleasure .
For the treatment of tumors of the vulva and vagina may also be used various forms of radiotherapy : the external one is used for cancer of the vulva also in order to reduce the size of the disease and to proceed with surgery less invasive , while for the tumor of the vagina external radiotherapy is often also accompanied by the internal ( brachytherapy , interstitial therapy , etc.) in which the radiation is applied directly to the diseased tissue .
In cases of more advanced disease , or when the removal of the tumor is not possible, one can make use of chemotherapy , usually systemic ( ie that is administered intravenously or orally and is directed to the whole body , not only to the tumor ) .
Finally topical treatments are available that consist of applying the chemotherapeutic drug ( fluorouracil ) directly on the skin in the region of the tumor and which is used especially in the case of pre-cancerous lesions , but not in the case of invasive tumors) and may also have given rise to metastases in distant organs .
Symptoms
The initial stages of cervical cancer are typically asymptomatic and most common symptoms often can be linked to other non-tumoral pathologies .
Among the warning signs that may raise suspicion of cervical cancer there are , for example, abnormal bleeding (after a sexual relationship between two menstrual cycles or menopause) , vaginal discharge without blood or pain during sexual intercourse.
Diagnosis
In recent years, the Pap test has been renovated and is especially changed the way we read the results that today is based on the so-called " classification of Bethesda ."
In practical terms this means that the gynecologist will give you the test results interpreted according to these new international standards , much more accurate than before.
If the Pap test is negative, the test can be repeated after three years, but if abnormalities are found , the doctor may prescribe additional tests , such as the search for HPV DNA or colposcopy .
This examination , which as the Pap test lasts a few minutes , is painless and is performed by the gynecologist at the clinic , is based on the close observation of the uterine cervix with a special microscope placed in front of the patient and also allows you to illuminate the region to be examined.
Before the observation , the gynecologist is the cervix with a solution of acetic acid which highlights any areas containing abnormal cells that can be directly taken with a special instrument .
Once the diagnosis of cancer of the cervix may be prescribed tests such as computed tomography (CT ) , magnetic resonance imaging or positron emission tomography (PET) to accurately determine the extent of the tumor .
How to care
The choice of treatment to be used for the treatment of cervical cancer depends mainly on the stage of disease at diagnosis , but is also based on other criteria such as for example, the state of health of the person , his age and his needs .
Often also proceed by combining two or more treatments to achieve maximum effectiveness.
Surgery is one of the possible choices and the type of operation varies depending on the spread of the disease . In the earliest stages , when the tumor is in a preinvasive stage , can be used cryosurgery or laser surgery using cold or a laser beam to freeze or burn diseased cells .
When the tumor is a bit ' more widespread, but still confined to a limited area of the cervix , the choice falls on the so-called conization , an operation in which a cone is excised tissue at the lesion without compromising the function of the organ and keeping open , for example , the ability to have children.
If the tumor is more extensive , you go to hysterectomy , an operation that involves the removal of the uterus , and in some cases you can even get to the removal of adjacent organs such as lymph nodes , fallopian tubes and ovaries. The mode of operation can be minivasiva or open surgery .
Today, with the aid of robotic laparoscopy is possible to perform the radical surgery necessary for this type of cancer, nerve spearing technique , with a reduction of the operative time , complications , and a better and more rapid recovery of functions.
Radiation therapy , which kills cancer cells with radiation , it is a valid treatment in some cases and totally painless , radiation can also affect well-defined areas that include the uterus , but also the adjacent areas in the event of widespread disease .
In addition to traditional radiation therapy in which the radiation source èesterna , exists today also brachytherapy , or the insertion into the uterus of small ova that emit radiation .
Both the external therapy is brachytherapy remain intact and do not alter the reproductive system in many cases the ability to have children .
A third option for the treatment of cancer of the cervix , but reserved the advanced forms or invasive , is chemotherapy : are administered intravenously different drugs against the tumor , often combined with each other , including cisplatin , paclitaxel , topotecan etcetera .
Who is at risk
One of the main risk factors for cervical cancer is infection with HPV , the human papilloma virus , which is transmitted through sexual contact.
That's why some measures that limit the possibility of infection ( condom use or vaccination ) are protective against this type of cancer while not 100 percent effective : the condom , for example, does not completely protect against infection since the virus can also be transmitted through contact with the skin regions not covered by the condom .
In contrast, early initiation of sexual activity and multiple sexual partners may increase the risk of infection , as well as immune failure that may be linked to several causes (eg, infection with HIV - the AIDS virus - or a previous transplant ) .
You still need to remember that not all HPV infections lead to cervical cancer . The majority of women who come in contact with the virus , in fact , are able to eliminate the infection due to their immune system without subsequent consequences at the level of health.
Finally, it is now established that only a few of the more than 100 types of HPV are dangerous from the standpoint of cancer , while the majority remains silent or merely give rise to small benign tumors called papillomas and also known as genital warts.
Other factors that may increase the risk of cervical cancer are cigarette smoking , the presence of close relatives in the family with this tumor (even if you have not identified the genes responsible for a possible hereditary transmission ) , a diet low in fruits and vegetables , obesity, and according to some studies, Chlamydia infections and a high number of pregnancies. In the latter case the reasons for the increased risk observed are still under study .
How widespread is
For a long time cancer of the cervix has been the most common form of cancer for women , but in recent years the picture has changed dramatically .
In developing countries , in fact, this cancer is still the second leading cause of cancer death , while in the Western world , the number of cases and the deaths continue to decline thanks to the introduction of the Pap test , a diagnostic tool early very effective.
In Italy every year a woman in 10,000 receive a diagnosis of cervical cancer in advanced form , but the chances of dying from this disease are less than one part per thousand .
Prevention
In most cases the cells that can lead to cervical cancer do not immediately give rise to cancer true , but they generate , initially , those that doctors call precancerous lesions.
These lesions are called CIN ( cervical intraepithelial neoplasia ) , SIL ( squamous intraepithelial lesion ) or dysplasia may progress slowly over the years to form the tumor . In fact , not all pre-cancerous lesions give rise to a tumor : in many cases , in fact, regress spontaneously without treatment.
However, it is beyond any doubt that prevent the formation of such injury or diagnose them and treat them early will dramatically decrease and almost eliminate the occurrence of cervical cancer in the population.
Limit the number of sexual partners and try to avoid relationships with people at risk are two tips for prevention , even if the winning strategy in this sense is based on regular gynecological check-ups .
During the visit , in fact , the gynecologist may perform a Pap test , a quick and painless test that helps identify pre-cancerous lesions in the initial stages , starting from the beginning of sexual activity, but no later than 25 years and at least until age 70 , all women should undergo this examination regularly once every three years , except in special cases .
There is also another test that can detect the presence of DNA of the HPV virus , but at the time of examination is recommended only in special cases by the physician after careful consideration of the case.
For some years now , in addition, women have access to another weapon against the human papilloma virus , a vaccine that can ward off the two types of HPV responsible for the majority of cervical cancers (HPV 16 and HPV 18 ) .
In Italy, the vaccine is now available free of charge to girls compimentyo at the age of 12 , but numerous studies are underway to evaluate the efficacy of vaccination in adult women with an active sex life and women have already come into contact with the virus.
READ ALL PATHOLOGIES



 Robotic surgery
Robotic surgery